The Provider Stabilization Fund
Colorado legislators can act now to protect access to care and stabilize critical health care infrastructure. Click below to read more about SB25-290 - Stabilization Payments for Safety Net Providers.


In 2024, an estimated 575,000 Coloradans lost their Medicaid coverage as pandemic continuous enrollment ended. Many are still eligible for Medicaid but unenrolled due to barriers or they are unable to afford private health insurance. Without this coverage, they are unable to access the health care they need. Providers who serve them across the state are seeing large increases in uninsured patients, creating significant financial burden. Additionally, health care providers are facing higher costs for supplies, prescription drugs and labor – and the Medicaid reimbursement they are receiving doesn’t cover the costs.
What you should know
about the Medicaid crisis in Colorado
1

Colorado is among the worst states in the country for disenrolling Medicaid members following the COVID crisis. Further, a significant portion of Coloradans who lost their Medicaid coverage did so for procedural reasons, not eligibility reasons - meaning they are being denied health care benefits to which they are entitled under federal law.
2

The loss of Medicaid coverage is driving increases in number of uninsured Coloradans seeking health care services. Losing coverage is devastating for vulnerable Coloradans and the increasing number of uninsured is financially unsustainable for the health care safety net that serves them.
3
This crisis impacts not only Medicaid clients and health care providers who serve them, but the broader Colorado economy, as Medicaid is a critical piece of the health care sector and health care is a major industry in our state and a critical employer, particularly in rural communities.
4
This is an urgent situation: If policymakers don’t act soon to stabilize the health care safety net and address Medicaid enrollment challenges, our state will lose critical health care infrastructure that will be costly, if not impossible, to rebuild.

Who we are
We’re a broad and diverse group of health care providers, consumer advocacy groups, business interests and local governments – stakeholders that are not always aligned on health care policy issues – who recognize the importance of stabilizing our safety net and ensuring Coloradans who are Medicaid eligible get the benefits to which they are entitled.
Coloradans tell their stories
Lola Milo is certain it shouldn’t be this difficult to make sure her family has access to the health care they need.
That’s because some months or several months in a row, she’s able to keep her family connected to Colorado’s Medicaid program. And then the letters come.
There’s one outcome of the challenges with Medicaid that stands out to Lisa Westhoff, a Regional Oral Health Specialist with Community Health Services in Aspen. One of her older patients recently lost Medicaid. He can’t afford co-pays available under Medicare. And he can’t understand why any of it is happening.
Kristin Boronski knows what the recent Medicaid retraction and changes to Medicaid reimbursements has meant for people who live in her small town of Basalt and all up and down the valley.
My name is Julianna Mascarenas, and I am here today as a single mother of six children, four of whom still live at home. I want to share how losing Medicaid has profoundly impacted our lives.

IN THE NEWS
Safety net providers in Colorado say they're losing millions of dollars a year due to uncompensated care and, without help, they'll need to close clinics.
The crisis has been building for years due to changes in Medicaid coverage and soaring health care costs.
Medicaid already accounts for one-third of the state's general fund budget and is increasing by $1.4 billion a year.
More than 5 million American children have lost their Medicaid coverage after states were required to recertify Medicaid recipients' eligibility. Procedural and paperwork issues were believed to be why many lost their coverage. NBC News' Jesse Kirsch reports on one father in Colorado struggling to get Medicaid reinstated for his young daughter.
DENVER (KDVR) — Colorado’s budget is facing a billion-dollar deficit this year.
The governor has proposed cuts in some areas for members of the state’s Joint Budget Committee to consider. One group that could be impacted urged lawmakers to find another way. Nearly 50 healthcare groups that do not always see eye to eye are all asking state leaders not to issue any cuts to Medicaid.
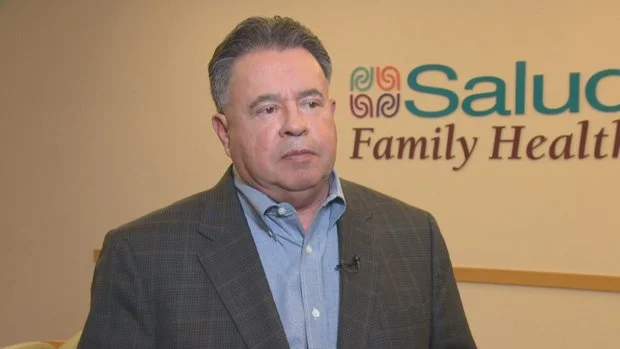
“It’s not a group that always agrees on all the health policy solutions. In fact, sometimes we very respectfully disagree on what the solution is. When it comes to Medicaid folks and the lowest income folks in Colorado, I think this coalition is very clear in knowing that we cannot balance our budget off the back of the poor and the vulnerable,” said Ross Brooks, Colorado Community Health Network CEO.
Over the last 15 years, Colorado voters and policymakers have prioritized health care coverage and access. We have worked together to ensure our neighbors could get the care they need when they need it. Our health care system is far from perfect, but Colorado’s progress has been undeniable.
Sadly, administrative failures in the Medicaid program over the last year have put that progress in jeopardy and created real hardship for Coloradans and our communities. We are now counting on our state partners in the Polis Ad-ministration and the General Assembly to step up in the next legislative session to strengthen Medicaid and support health care safety net providers.
In the 2022 legislative session, Colorado lawmakers passed a measure to review Medicaid provider payments more frequently as part of a broader push to boost health care worker pay at a time of widespread staffing shortages.
The measure, Senate Bill 236, ramped up the review timeline for dozens of publicly funded health care services to every three years from five, a move meant to enable the state to respond more quickly to medical providers facing financial crises.
Federal cuts to Medicaid could further strain fledgling finances, they say.
A group of health care organizations on Tuesday joined together to call attention to an issue that they said could get worse in 2025.
Many Coloradans no longer have Medicaid coverage due to the unwinding of a pandemic-era mandate that kept them enrolled in the program. At the same time, the state's health care leaders say they fear the new presidential administration plans to further cut Medicaid or other health program funding.
The combination could prove unsustainable for health care providers, who rely in part on Medicaid reimbursement to pay for the services they provide and who are already feeling financial pressures, they said.
The Eagle River Valley is an incredible place to live for many reasons — natural beauty, outdoor recreation, and a strong sense of community, to name just a few. But for years, we have struggled with a cost of living and compensation imbalance that has made health care coverage tenuous at best for many of our neighbors.
Because of this, Medicaid is essential to the health of our community. Emerging from the COVID-19 crisis, our local health system is facing new challenges that have reached a crisis point.
The Roaring Fork Valley is an incredible place to live for many reasons — natural beauty, outdoor recreation and a strong sense of community, to name just a few.
But for years, we have struggled with a cost of living and compensation imbalance that has made health care coverage tenuous at best for many of our neighbors. Because of this, Medicaid is essential to the health of our community. Emerging from the COVID-19 crisis, our local health system is facing new challenges that have reached a crisis point.
For more than two decades, Colorado has invested in the health care safety net because we know that access to health care is a primary path to financial security and quality of life for Coloradans and a healthy, vibrant state for all of us. But over the last year, as we have emerged from the COVID crisis, Colorado has failed our neighbors on Medicaid and jeopardized the safety net health care providers who serve them.
Two more community mental health centers are eliminating jobs and cutting programs as Colorado’s safety-net health system staggers from a massive drop in Medicaid rolls.
WellPower, which provides mental health care in Denver regardless of whether patients have insurance, is cutting six positions from its co-responder team that pairs social workers with city park rangers, fire and law officers. It’s also eliminating its virtual therapy program, which connected 579 patients with therapists online last year. And it’s ending its lease of Garfield House, an apartment complex where the mental health center has placed patients who needed housing.
Larimer County’s community mental health center has abruptly laid off 75 employees, causing a gap in care for some of the most vulnerable patients and increasing concerns about how far the fallout will spread after a seismic shift in Medicaid funding.
Connor Grogan had 35 clients at SummitStone Health Partners in Fort Collins when he was told at a mandatory meeting last week that he was among those losing their jobs because of a budget crisis. He had to turn in his phone and laptop on the spot, with no opportunity to say goodbye to his patients.
Colorado stands out among the 10 states that have dropped the highest share of Medicaid enrollees since the U.S. government lifted a pandemic-era restriction on removing people from the health insurance program.
It’s the only blue state in a cluster of red states with high withdrawal rates – a group that includes Idaho, Montana, Texas, and Utah – in the Medicaid "unwinding" underway since spring 2023.
One of Montana’s largest health clinics that serves people in poverty has cut back services and laid off workers. The retrenchment mirrors similar cuts around the country as safety-net health centers feel the effects of states purging their Medicaid rolls.